Clinic Hours
MonclosedTue12 - 7 pmWedclosedThu12-7 pmFri2 - 7pmSat9am - 1pm
- Success Stories
Highly recommend Frank Grill and staff. They are very friendly, the place is clean and best of all, they helped cure my ailments. First, he helped with my sciatica and lower back pain, then a few months later, he helped with my stress. If you’re new to acupuncture and on the fence, you can’t go wrong. Give it try! Five stars to Frank and staff.
Dr Frank knows what he is doing and has helped me more than physical therapists, back doctors, especialists and chiropratics combined together over the years. He really cares for his patients. LikeAfter much skepticism, my sister convinced me to come here and give acupuncture a go back at the end of August.
I suffer from PTSD and this manifests itself as debilitating depression and anxiety. This in turn made every day of my life miserable for as far back as I can remember. I was constantly on edge and lashing out at people I love almost on a daily basis. I suffered from phantom pains all over my body and always
... Read more »
Acupuncture
What Are The Acupuncture Points?
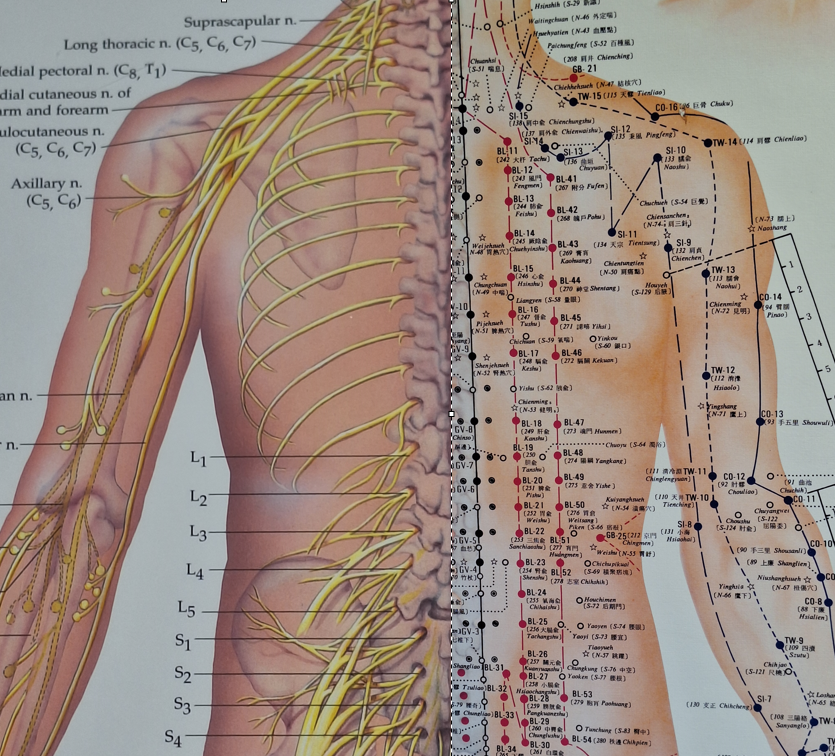
Spinal Nerves (Left) Versus Meridians (Right)
If there is one thing that is said to me, over and over again, it is: “I don’t like needles.” If there is another thing that is said to me over and over (and over) again, it is: “How does acupuncture work, scientifically?” In clinic, I endeavor to answer this question, but because time is limited and the subject is complex, I feel there is rarely, if ever, a successful understanding of this topic created. So, after many, many years, I decided to give this question the answer it deserves.
If you have had acupuncture before, at some point you probably noticed your acupuncturist had colorful charts on the wall depicting the classical acupuncture point locations. These points are linked one to another by a series of lines called “meridians,” or channels. In Traditional Chinese Medicine thinking, these lines represent an energetic connection between points.
According to traditional theory, your body’s vital energy, or “qi” flows along these lines. If your state of health is good, the qi flows smoothly. If qi is blocked by trauma, stress, poor diet, or environmental factors, it slows, or stagnates, resulting in symptoms. It is considered the job of the acupuncturist to locate these blockages and remove them by stimulating the acupuncture points, usually with needles.
Many people will accept this conception. Intuitively, it makes sense, and it resonates with the metaphor of waterways or traffic flows. However, some people will balk as they consider this explanation to be unscientific. And truth be told, they are correct! In our western scientific paradigm, there are various units for measurement of different types of energy. If qi is a form of energy, there should be a way to measure it. There is none.
Do the acupuncture points and meridians represent nodes of energy and connections in between them? In my opinion, no. Certainly, these points have significance, which I will explore below, but the science of energy is physics, and the sine qua non of physics is measurement, and qi cannot be measured. Which is not to say there is no energy flow in the body, in fact there is constant movement of thermal, chemical, and electrical energy. One way to explain Qi may be to consider it an aggregate of these processes. However, there is no singular defining characteristic of what qi is relative to other forms of energy.
How were these points discovered? It is unclear, lost in the haze of the past. It is certainly possible that the ancient Chinese mapped these points empirically, through palpation and trial and error. Perhaps they realized the physiological significance and treatment utility of stimulating these points, but did not fully understand the mechanism of action. It is possible they crafted a system of explanatory value that was internally consistent and useful, but does not correspond to modern anatomical understanding. I believe this is the case.
But the question remains: if the acupuncture points are not conduits for qi energy, then what are they? And why does it matter? It is still possible to utilize the meridian system for diagnosis and treatment, and many Traditional Chinese Medicine (TCM) trained acupuncturists do. However, there are several problems with this approach. One, the terminology of TCM alienates western trained healthcare professionals. This is why the concept of “dry-needling” has been so successful. By retaining the techniques of acupuncture and repackaging the conceptual framework, it is much more palatable to the medical community. (As an aside, It is somewhat bittersweet to me after many years of having my treatment rejected by science minded individuals, to watch it become enthusiastically embraced by the physical therapy community as the newest and hottest method around. There is a lesson for myself and my profession here, but that’s for another time).
The second limitation is that it limits refinement and growth. Traditional Chinese Medicine is a canonical medicine, meaning it is based on the classics. Characteristics of acupuncture points are handed down as “statements of fact,” immutable axioms. On the one hand, there is a high degree of value in this, as the past represents a rich store of knowledge. On the other hand, it can inhibit new approaches. New discoveries in anatomy and physiology can form the basis for new techniques, and they often are. For example, scalp acupuncture based on fMRI of brain activity has become quite popular. This approach has little reference to the classical acupuncture paradigm. Of course, dry needling replicates acupuncture techniques with no incorporation of meridian concepts whatsoever. The success of these methods call into question the relevance of the traditional conceptual framework.
We still have not answered the question of what the acupuncture points are. Various explanations have been proposed. In the dry needling community, it is largely (but not completely) accepted that they are myofascial trigger points. Myofascial trigger points represent areas within muscles that are prone to fatigue and accumulation of metabolic waste. They are tender to palpation and often will radiate pain in a predictable pattern when pressed. These patterns often correspond to acupuncture meridians. The myofascial trigger points as mapped out by Dr. Janet Travell do indeed have a high degree of correspondence with the acupuncture points.
Other people such as Dr Helene Langevin have proposed that the acupuncture meridians represent fascial planes. Some acupuncturists have latched on to more obscure concepts, such as “Bonghan ducts.”
It is beyond the scope of this article to detail the pros and cons of each of these approaches. However, in my opinion, the most likely and most obvious explanation is that the acupuncture points represent nothing other than areas of neuroanatomical significance.
I first noticed this many years ago when comparing a chart of the peripheral nervous system side by side with an acupuncture point chart. The meridians were too close to the nerves to be coincidental, yet at the same time they were not completely aligned. My opinion was confirmed when I started studying the work of Dr. Poney Chiang. According to Dr. Chiang, research to investigate the anatomical significance of acupoints systematically began in 1959 at the Shanghai First Medical College. Their research showed that the acupuncture points have a very high degree of coincidence with areas of neuroanatomical relevance.
For example, 323 of 324 acupoints are associated with peripheral nerves. 93.83% are associated with superficial cutaneous nerves, and 52.5% are associated with deep nerve trunks. Additionally, in experiments, using nerve anesthetic techniques removed the effectiveness of acupuncture points, suggesting that their function is based on neurology, not on unseen energy circulation.
What are the implications of this? It means that the acupuncture points are nothing other than areas to access the nervous system for stimulation, and that the needles (combined with electrical current), are a vector for achieving that stimulation. It also means that optimization of the acupuncture treatment requires a thorough understanding of the nervous system.
The nervous system is divided into the central nervous system (brain and spinal cord), and the peripheral (nerves extending from the spine into the limbs). The three types of nerves are sensory, which provide
sensation, motor, which activate muscles, and autonomic, which are further divided into sympathetic and parasympathetic, which have various stimulating or sedating effects on the organs, circulation, glandular secretion, etc. What the meridian system gives us, when properly interpreted, is nothing less than a road map to normalizing various functions within the nervous system. Through this system, you can modulate pain, but also remove motor inhibition (increase movement), and normalize autonomic (organ) function.
Think of how remarkable this really is!
What does this mean for you? Most acupuncturists have some familiarity with this concept, but many remain in the traditional paradigm. Some utilize this framework, but very few explore the depths of neuroanatomy this approach necessitates. To get good results with this methodology requires a commitment of constant study and research. It requires a rigorous clarity of diagnosis and a specificity of technique.
In my opinion, however, it is worth it. Using a neurologically based approach to acupuncture produces an accuracy in results not obtainable with traditional thinking. As well, allows integration by using the common vocabulary and concepts of biomedicine. (Sometimes I am a little saddened when I think of all the people I’ve met who rejected acupuncture because they believed it had no scientific basis.) Finally, it opens the door to innovation, allowing research from other modalities, such as clinical neurodynamics, anesthesiology, and electromedicine to be seamlessly integrated into acupuncture practice. This can do nothing but benefit our patients.
For me personally, this does not erase the TCM meaning of the point, rather it enhances it. Hopefully, you now have some deeper understanding of what acupuncture is. In future articles, I will explore the actual mechanisms of action of needling with electricity and how it can be used to benefit you.
TLDR: Acupuncture points and meridians are really nerves, and acupuncture stimulates nerves to relieve pain and improve function.
Case Study – Piriformis Syndrome
“Sciatica” is one of the conditions people seek acupuncture treatment for most frequently. As you will say in the case below, most of the time it is not actually sciatica which people are experiencing. I have prepared the following case study for you in order to give you an idea of how we evaluate and treat such pain with acupuncture. I hope the insight it gives you provides you with the confidence to seek treatment if you are suffering from this type of pain.
Case Study – Sciatica or PIrifomis Syndrome?
A 28 year old male came to the office on a Saturday with pain in the left posterior hip. The pain had begun several days earlier while working (physical labor). He had a strong ache in posterior hip with a radiating sensation down the leg. Additionally, the sensation made him feel anxious and uneasy, causing difficulty sleeping. Ibuprofen helped it only slightly. He had diagnosed himself with sciatica.
What Is the Sciatic Nerve?
The sciatic nerve is composed of nerve roots from the L4, L5, S1, S2, and S3 vertebrae. They merge to form a single, large nerve which exits under a bony arch called the sciatic notch. The sciatic nerve runs through the pelvis, travelling under the piriformis muscle before heading down the back of the leg.
It separates into two branches at the back of the knee to form the tibial and peroneal nerves, which supply the lower leg and foot. The sural nerves branch off from the tibial and peroneal nerves, terminating in the foot.
The sciatic nerve provides motor input for bending the knee, bringing the thighs together (adduction), and flexing and extending the ankles and toes. It conveys sensation from the back of the thigh, the entire lower leg, the ankle, and the sole of the foot.
Sciatica Vs. Pseudo-Sciatica
Many people experience the symptoms described above and identify it as sciatica. In reality, most of the time they are experiencing “psuedo-sciatica.” What is the difference?
True sciatica is a set of symptoms caused by irritation or compression on one or more spinal nerve roots in your lower spine, not the sciatic nerve itself. This could be due to a herniated disc or spinal stenosis,. The nerve roots which merge together to form the sciatic nerve are under pressure. This is a form of radiculopathy. (Radix is a Latin term meaning root, and pathos is a Greek term for disease).
In reality, what most people are experiencing is a form of muscular tightness, called piriformis syndrome. In this case, the sciatic nerve is directly irritated or compressed by your piriformis muscle, deep in your hip. The symptoms of piriformis syndrome may affect the buttock and hip, as well as traveling down into the thigh and leg.
What is the Piriformis?
The piriformis muscle originates at the sacrum (the flat bone beneath your spine in the center of the pelvis) and attaches to a bony knob (the greater trochanter) on the femur (thigh bone) on the outermost part of the hip.
The function of the piriformis is to externally rotate and abduct the hip. This means turning your hip outward and bringing your thigh outward to one side while your hip is bent. This happens when raising your knee and bringing your leg out when getting out of a car (which can be one of the painful movements when it is inflamed). It is also involved in walking, running and standing.
Causes of Piriformis Syndrome
Ordinarily, the sciatic nerve is directly underneath the piriformis. Occasionally, people have an atypical anatomical variation. Sometimes, the sciatic nerve passes directly through the piriformis, which can lead to piriformis syndrome. More commonly, there is inflammation of soft tissues, muscle spasm or both, causing nerve compression.
This can happen with direct trauma such as a car accident or a fall. However, it is most likely the gradual tightening of the piriformis muscle is due to poor posture and overuse. Activities, such as long distance running or prolonged standing without proper stretching and strengthening of piriformis muscle will contribute to piriformis syndrome. However, in my experience, people who sit for a long period of time with poor posture, especially drivers, seem to suffer from this the most.
Symptoms of PIriformis Syndrome
Symptoms of piriformis syndrome can be variable. Some of the common symptoms include:
- Pain in the opposite sacroiliac joint
- Pain with sitting standing or walking for more than 20 minutes
- Intense pain while sitting
- Sensation of pins and needles, numbness, burning, tingling, or itching down the back of the thigh, usually stopping above the knee
- Pain improves with movement
- Pain when moving from sitting to standing
- Foot numbness
Differentiation: Sciatica VS. Pseudo Sciatica
One way to tell is to consider WHERE the pain is felt:
- In piriformis syndrome, buttock and hip pain is typically more common than lower back pain.
- In sciatica, the leg pain is usually greater than lower back pain and the pain may extend below the knee. The affected leg may also feel heavy.
Another way to tell, is the effect of MOVEMENT
- In piriformis syndrome, the pain typically increases while sitting for long periods of time and/or during hip movements.
- In sciatica, raising the affected leg while lying down (while keeping the other leg straight) may induce pain.
Evaluation
The primary physical test for sciatic like symptoms is the Straight Leg Raising (SLR). The straight leg raise places stretch on the sciatic nerve as it passes through and around the structures of the pelvis and traverses down the posterior aspect of the thigh. The straight leg raise test is performed with the patient on their back. The examiner gently raises the patient’s straight leg, and the test is considered positive when the patient experiences pain along the lower limb. In this case, the test was negative (which is good).
The patient was walking with an antalgic gait. Muscle testing revealed weakness at the gluteus medius (resisted hip abduction) and the tensor fascia latae. Palpation revealed extremely tender points at the piriformis and gluteus medius.
Treatment
The purpose of the physical exam is to identify areas of muscle tension and weakness. Acupuncture points are selected based on their neuroanatomical relevance. The majority of points chosen are motor points. Motor points when stimulated, especially with electrical acupuncture, can normalize the tension in a given muscle. This, in turn, reduces pressure on the underlying nerves and gives pain relief.
Acupuncture was given in the first session to the following points. The points are given with their acupuncture nomenclature, as well as the important anatomy they reference.
GB-29 : Motor Point of Tensor Fascia Latae
GB-30: Motor Point of Piriformis.
UB-53: Superior Gluteal Nerve: innervates Gluteus Medius, Gluteus Minimus and Tensor Fascia Lata.
UB-54: Inferior Gluteal Nerve: innervates Gluteus Maximus.
UB-37: Descending Branch of Posterior Femoral Cutaneous Nerve/Biceps Femoris Motor Point
UB 57: Lateral Head of Gastrocnemius Motor Point
The superior gluteal nerve was connected to the lateral gastrocnemius motor point for 10 minutes of electrical stimulation. Then gua sha was performed to the posterior hip and thigh. Upon standing, the patient felt better but still had some pain in the anterior aspect of the thigh. So treatment was performed to the following points:
ST-31 : Upper Rectus Femoris Motor Point
ST 32 : Lower Rectus Femoris Motor Point
These points were connected with .5 hz electrical stimulation for 10 minutes.
After the treatment, the patient had complete relief. The relief lasted for several hours, upon which the pain came back, but not as severe. The patient required ibuprofen later that night, but by the next day the pain had abated substantially. Upon return to work on Monday, the patient was able to work with some restriction. On Tuesday, we had a follow up visit. The pain was mostly resolved, we performed a treatment similar to the first, and the patient was released with a simple exercise to do at home for prevention.
Discussion:
It is important not to just treat the painful areas, but also muscles that contribute to movement of the leg and back as a whole. In addition to the piriformis itself, the Gluteus medius (the hip abductor) and tensor fascia latae are almost always a part of the treatment. In this case, it was also necessary to treat the hip flexor. These areas of weakness can be uncovered by careful exam.
Also of note, the acupuncture points are selected based on what neuroanatomical structure they relate to, versus the traditional selection of points based on meridians. This, in the author’s opinion, creates an approach which is both more reasoned and more accurate.
Not every case resolves so quickly and easily. The chronicity of the condition, structural imbalances, age, and diet all play a role. In some cases, Chinese herbal medicine such as Du Huo Ji Sheng Tang is added. However, most cases can at least improve if not be totally resolved with acupuncture and Chinese medicine treatment.
Acupuncture Vs. Dry Needling: What You Need to Know
“Have you heard of dry needling?”
“My physical therapist wants me to try dry needling. Should I?”
“What is the difference between dry needling and acupuncture?”
Have you heard of dry needling yet? Maybe you have heard about it from your doctor or physical therapist. Perhaps you have friends who have experienced it and they have suggested you try it. It’s different than acupuncture! Maybe you know it involves acupuncture needles. If you’ve seen it, it looks like acupuncture, but it’s not acupuncture. Or is it?
There’s been a lot of confusion around this topic for the past several years. So, at long last, I decided it is time to clarify the differences and similarities of what acupuncture and dry needling are. Since I am an acupuncturist, let’s first take a quick look at what acupuncture is, and then see how dry needling fits into the picture.
What is Acupuncture?
Acupuncture finds its historical roots in ancient China. Acupuncture first made it’s way to the US in the form of TCM, or Traditional Chinese Medicine. Acupuncture uses stainless steel, sterile needles to stimulate areas within the body. The purpose of acupuncture is to relieve pain, reduce stress, and improve function.
How does acupuncture work? Here is where it begins to get tricky. We have a traditional understanding of how acupuncture works (which some acupuncturists still use today), and a modern understanding of how acupuncture works (which is what I use in my practice). What is the difference and why does it matter?
In the traditional understanding of acupuncture, the body is considered to have a vital energy. This vital energy, or “Qi” flows along lines called meridians, This energy can become stuck due to trauma, overuse, or stress. This energy stagnation can result in pain and dysfunction. Stagnation can be relieved by stimulating acupuncture points along the meridians. The acupuncture points can be located where the pain is, or the can be located in other parts of the body, such as the ear, hand or foot.
The modern understanding of acupuncture, on the other hand, is concerned primarily with muscles and the nerves which supply them. From this perspective, treatment is given to “trigger points,” or knots which form in the muscles. The trigger points also form due to stress, trauma or overuse. Placing the needle in the trigger point causes the muscle to fasiculate, or “twitch,” which is usually followed by profound relief of pain and stress. The action of causing the muscle to twitch with a needle is also what is called “dry-needling.”
Why is it important to understand these two concepts? Because dry needling is nothing other than doing acupuncture according to the modern understanding. This is the conceptual framework used by physical therapists, chiropractors, and even some acupuncturists (including myself).
In other words, ALL dry needling, IS acupuncture. But not ALL acupuncture is dry needling. Put another way, dry needling is just one technique, or method, of acupuncture. The physical therapist has access to this technique, but not ALL the styles of acupuncture. There are very effective acupuncture styles which involve putting needles in locations far away from where the pain is, Which means, SOME acupuncturists will treat you in a similar fashion to a physical therapist, and some will not.
Confused yet?
Pros and Cons
The first question that springs to many people’s minds is, “Which is better?” The better question is: “Which is better for me?” Traditional acupuncture or dry needling both need to fit into a comprehensive treatment plan. A good clinician always starts with evaluation, questioning, examination, and diagnosis. These should all come before any technique is decided upon. I use my clinical experience to determine which acupuncture technique is going to best serve the person in front of me. Sometimes dry needling is absolutely the best thing I can do for them. Sometimes a traditional technique is better. Most often, I mix and match using 2 or more styles to come up with a combination that fits the unique individual.
The pros of the dry needling technique are that it can very often produce extraordinary pain relief, quickly. The cons are, it can be uncomfortable initially, and sometimes can produce soreness for a day after treatment. Additionally, some conditions can be aggravated by it. My approach has always been to carefully choose when to use it, and start slowly to see how much a person is comfortable with, and increase over time. This has produced the best results for me.
Should You Try Dry Needling?
Many people have recently learned about dry needling and are eager to try it, understandably so. I first began the dry needling approach in 1999. Chances are, if you have been my patient, you have already had dry needling. If you have ever felt the muscle “twitch” during treatment, you have had dry needling. (If you ever heard me talk about the muscle locations or the “green triangles,” you know what I am talking about). Until recently, I just called it “acupuncture.” No one knew the difference. But today, with the increased awareness of different healing techniques, I take the time to indicate when we are using this method.
If you haven’t been in for awhile, and would like to experience this fabulous technique, give us a call today. one of the wonderful things about acupuncture is that there is always more to learn, and I am constantly finding new ways to better serve you.
Also, if any of you have any questions, give us ac call today! I am always happy to answer your questions.
What Is The Exstore System?
Greetings and happy holidays! I hope this finds everyone well. I have some exciting things to share with you. This year I celebrated my 15th(!) year in practice. It seems hard to believe. Persisting in anything for 15 years is a challenge. One of the things that keeps my going is the constant search for newer and more powerful acupuncture techniques. I have traveled around the country, gone to endless seminars, and read dozens of books. Acupuncture is a huge field and there are many, many styles to choose from. There are many Chinese styles, but also Korean, Japanese, Vietnamese, and even western style or “dry-needling.” I have explored many of these but over the years I came to rely on the treatment of “trigger points” as a primary tool.
The trigger points (or “knots”) in the muscles are the source of a great many pain problems. For years, I have studied trigger points and how to release them. Many of you are familiar with the acupuncture trigger point techniques I have used and the profound relief they can provide. Getting the muscle to twitch or “jump” (sometimes referred to as dry-needling) can release tension and pain instantly.
As good as these techniques are, I am always on the lookout for ways to make them better. To find a way to make them faster, more accurate and more powerful. I constantly research and test new methods. Some work ok, some are so-so, but rarely do I find something that blows me away. I can honestly say finding the EXSTORE system was a game-changer for me.
In the past several months, we have introduced the EXSTORE method of assessment and treatment. Those of our patients who have experienced this technique have been very happy with the outcomes thus far and we are excited to tell you about it. In 15 years of practice, nothing else I have found has made such a huge difference.
The EXSTORE system is a method of assessing pain patterns quickly and finding the root cause. Basically, we test the strength of the muscles to find which ones are neurologically inhibited (weak). These muscles are not doing their job of supporting the body structure and can lead to pain and dysfunction. After pinpointing which muscles are weakened, we apply acupuncture plus electric stimulation (similar to a TENS unit), which immediately “wakes up” the muscle, changing the strength instantly! When the muscles are reawakened, the body will be able to move better and the painful situation will improve, often dramatically.
The EXSTORE technique is combined with all the other methods we have, including cupping, gua sha, kinesiotaping and others. However, it is now the foundation on which these other techniques rest. This combination has produced much better results than I have had previously, for sciatica, neck pain, knee pain and many other common conditions. It even works great for IBS, PMS, and other internal complaints. If you have not experienced this technique I invite you to call today at 630-369-3237 and give it a try!
Allergies Relieved by Acupuncture in Study
Allergies Relieved by Acupuncture in Study
It’s summer and that means it’s time for fun… and allergies! There is good news though! Allergy sufferers who received 12 acupuncture sessions had fewer symptoms and required less antihistamine medication compared to a control group, as reported in Annals of Internal Medicine.
Seasonal allergic rhinitis, commonly known as hayfever, is usually a result of allergies to plant pollen. Stuffy nose, itchy eyes, and sneezing are the familiar foes of spring and summer. For some people, antihistamines offer relief. For others, the side effects of antihistamines (dry mouth, drowsiness, dizziness) make them unappealing. For others, they simply don’t work. Increasingly, people are turning to acupuncture for relief of allergy symptoms.
Led by Dr. Benno Brinkhaus, researchers from Charite-University Medical Center, in Berlin, Germany, randomly selected 422 volunteers. All hay fever sufferers, they were divided into three groups.
Twelve treatments were administered over eight weeks in the first year. Patients in all three groups were allowed to take antihistamine medication whenever their allergies worsened.
The results showed that those in the acupuncture group reported better improvements in their symptoms over the eight-week period of treatment, as well as needing fewer antihistamine drugs, in comparison to the other groups.
Eight weeks of ending their treatment, the benefits of the acupuncture faded. However, Dr. Brinkhaus, a medical doctor and acupuncturist, said that does not necessarily mean that the benefits of acupuncture have been eliminated.
Our experience at Naperville Acupuncture Center is that people do benefit from receiving acupuncture for allergies. On average, we treat people once or twice per week during the peak allergy season. Some people also receive and herbal formula. The symptoms and frequency of allergies are diminished, and the need to take medication is reduced. However, allergies are not permanently eliminated. Call today to find out how we can help you!
